Neck Trauma : Cervical Spine Injuries
Cervical spine injuries can occur when sufficient force is applied to overcome the musculoskeletal and/or bony integrity. Examples of events which apply these strong forces are: motor vehicle accidents, in hard contact sports, after a fall, or by hitting your head against a hard surface, such as when diving into a shallow pool, or having an object hit your spine. These accidents can cause injuries that range from mild cases of neck pain, called whiplash, to injuries that can cause paralysis and/or numbness of the rest of the body below the level of injury. See below a list of categories that contribute to Neck trauma.
Whiplash
Whiplash occurs when a forceful impact (commonly from behind) causes your head and neck to snap forward and back in an abrupt, violent motion. It is commonly seen in car accidents and contact sports.
Whiplash (also called cervical hyperextension injury or flexion-extension neck injury) refers to an injury to the soft tissues of the neck including the ligaments, tendons, and muscles. The symptoms of whiplash include neck pain and stiffness. Upper back and shoulder pain can also occur. Most whiplash injuries heal within weeks, but if left untreated they can linger and turn into chronic conditions that last for years and lead to pain and sometimes disability.
Disc Prolapse
(See Abnormal Spinal Anatomy section)
In the event of a traumatic force, some of the soft disc material breaks through the fibrous tough outer lining. This loose fragment or bulged disc material will extrude out to the side of the spinal canal and impinge on the exiting nerve root at the lower level (e.g. C6 at C5-C6). This may result in arm or hand pain and/or numbness (commonly referred to as Cervical Radiculopathy).
If the space for the nerve root (foramen) is already compromised because of associated disc space collapse or bone spurs (osteophytes), the added impingement of the disc may irritate the nerve root and cause a radiculopathy (arm pain). If the foramen is not compromised, the radiculopathy may be temporary and relieved with conservative treatment.
Herniated cervical disc treatment options
In general, most cervical disc herniations or cervical radiculopathy will heal with time and conservative treatment and will not require surgery. The following includes an overview of:
Conservative treatments for cervical radiculopathy
As in the lumbar spine, the first line or treatment is generally a couple days of rest and non-steroidal anti-inflammatory drugs (NSAID’s).
If the pain is severe and/or continues for more than a couple of weeks, oral steroids can be useful to decrease inflammation. Oral narcotic agents can be added for severe pain, but should only be taken for a short time (less than two weeks).
If the pain lasts for more than two to four weeks, conservative treatments may include:
Physical therapy for exercises to help relieve the pressure on the nerve root
Chiropractic treatments for manual manipulation to help relieve the pressure on the nerve root
Manual traction to help open up the cervical foramen where the nerve root exits the spinal canal. If this therapy helps relieve the pain, a home traction unit can be prescribed. Traction should be initiated under a physical therapist's supervision.
For pain that does not get better with medical and physical treatments, epidural injections or peri-radicular blocks may be considered. Epidural injections effectively relieve pain approximately 50% of the time, and if they do work they may be repeated every two weeks up to a total of three times within one year.
Cervical radiculopathy (herniated cervical disc)surgical treatments
If 6 to 12 weeks of conservative treatment fails to relieve the arm pain, then surgical removal of the disc may be reasonable.
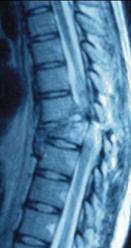
An MRI scan or CT with myelogram can confirm the presence of a disc herniation and the level that is affected. If the patient’s symptoms and neurological deficit match the results of the scan, surgery is reliable in terms of relieving arm pain and has a low complication rate.
The disc may be removed from the back of the neck (posterior approach) or from the front (anterior approach). Generally, surgeons favor the anterior approach for most cervical disc herniations.
Anterior surgical approach for a herniated cervical disc – may be favored if there is any disc space collapse, as the approach allows the surgeon to "jack open" the disc space and place a bone graft to keep it open. This procedure opens up the foramen, which gives the exiting nerve root more room
Posterior surgical approach for a herniated cervical disc – may be favored for a large soft disc that is lateral (to the side of) the canal
Both spine surgeries can usually be done with a short hospital admission.
Cervical spine fractures/dislocations
C1 Fractures- Atlas fractures
Incidence: 4% of cervical spine injuries
site:
posterior arch
anterior arch
massa lateralis
Jefferson fracture
Associated with:
fractures of C7 (25%)
fractures of C2 pedicle (15%)
Jefferson fracture
Burst fracture of atlas (C1)
widened lateral masses of C1 on open-mouth odontoid view
vertical compression injury
unstable
C2 Fractures- Axis fractures
incidence: 6% of cervical spine injuries
associated with atlas fractures in 8%
hyperflexion injury:
Odontoid fracture
Type I
-avulsion of tip of odontoid (5-8%)
-difficult to detect
Type II
-fracture through base of dens (54-67%)
-complication: nonunion
Type III
-sub dental injury (30-33%)
-prognosis: good
DDx:
os odontoideum
ossiculum terminale
hypoplasia/aplasia of dens
Hyperextension injury: hangman's fracture
Hangman's fracture
bilateral fracture of pedicles of axis (C2)
3 types (1-3)
Usually non surgical treatment for Type I, but surgery is Usually required for Type II and III
Sub-Axial Fractures
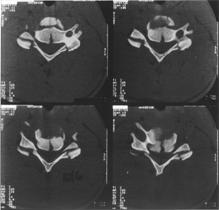
Burst Fracture
Burst fractures result from axial loading most often secondary to motor vehicle accidents and falls
The axial load drives the intervertebral disk into vertebral body below
Usually produces a comminuted, vertical fracture through the vertebral body
Fragments may be retropulsed into the spinal canal injuring the cord
Burst fractures, however, can have associated injury to the posterior ligamentous structures, especially if there is a combination of axial loading and flexion at the time of injury
Burst fractures may resemble hyperflexion teardrop fractures.
In a classical flexion-teardrop fracture, there is an avulsed anterior, inferior triangular bony fragment that is separated from the body and displaced anteriorly
Both the anterior and posterior ligamentous structures are injured, which may not be the case in a burst fracture
Tear drop fracture
Avulsion of anterioinferior corner of cervical vertebral body by anterior ligament
most severe and unstable injury of the C-spine
often the result of diving into shallow water
may be secondary to hyperflexion or hyperextension typically at C2
Usually associated with severe neurological compromise
Will usually require surgery (probably front and back procedures)
Clay shoveler's fracture
Avulsion fracture of spinous process of C7 or T1
sudden load on a flexed spine
may occur secondary to rotational injury
sudden load on a flexed spine
Cervical Dislocations
A displacement of spinal vertebrae in the neck, so that adjoining bones no longer touch each other. Subluxation is a minor dislocation. Joint surfaces still touch, but not in normal relation to each other. Neck subluxation followed by spontaneous reposition occurs frequently in athletes. A neck dislocation is a serious injury that can lead to spinal-cord damage and paralysis of all four extremities, and sometimes leads to death.
Body Parts Involved
Vertebrae of the spine in the cervical (neck) region.
Ligaments that hold the vertebrae in proper alignment.
Cartilage between the vertebrae that cushions the bones.
Spinal-cord and nerve roots (sometimes).
Causes
Forceful flexing, extension or rotation of the neck.
Direct blow or violent force on the neck or head.
End result of a severe neck sprain.
Can be at C1/C2 (Cock-Robin appearance, wry neck)
or below C2, either unifacet (1 joint) or bifacet (both joints).
May cause serious neurological damage to the spinal cord
Needs Neurosurgical advice +/- surgery
Spinal Cord Injury
Injury to the spinal cord in the neck causes a condition known as tetraplegia or quadriplegia. These terms mean exactly the same thing, one is a Greek term and the other is Latin.
There is injury to the spinal cord between the spinal cord segments C1 and T1.
This causes paralysis and loss of feeling involving all 4 limbs as well as the bladder, bowel and sexual organs.
Paraplegia
Injury to the spinal cord below the neck causes paraplegia. There is injury to the spinal cord below the T1 cord segment. This causes weakness and loss of feeling in the trunk, legs and bladder, bowel and sex organs. But the arms and hands are normal.
Level of injury
We describe the level of the injury by referring to the last spinal cord segment where the movement and feeling are normal.
For example, if your injury is called “C5” this means that you would be able to bend your elbow normally and would have normal feeling to around the level of your elbow but below that the movement and feeling would be reduced.
Incomplete
An incomplete injury is one in which there is some movement or feeling below the level of the injury or in the genital region.This implies that the damage in the spinal cord does not involve the whole spinal cord and that some messages are getting past the area of damage.
The chances of improvement and recovery are better if the injury is incomplete.
Complete
A complete injury is one in which there is no movement or
feeling in the genital region.
This means that the damage in the spinal cord involves the whole spinal cord and no messages are getting past the area of damage.
The chance of improvement and recovery if the injury is complete is much lower.
if pressure is applied to the spinal cord or
if the blood supply (which brings the oxygen to the cord) is cut off for more than about 15 minutes.
spinal cord damage is probably due to a combination of both factors.